This information is intended for US healthcare professionals. For educational purposes only. By clicking the button below, you certify that you are a US healthcare professional.
I am a US healthcare professional



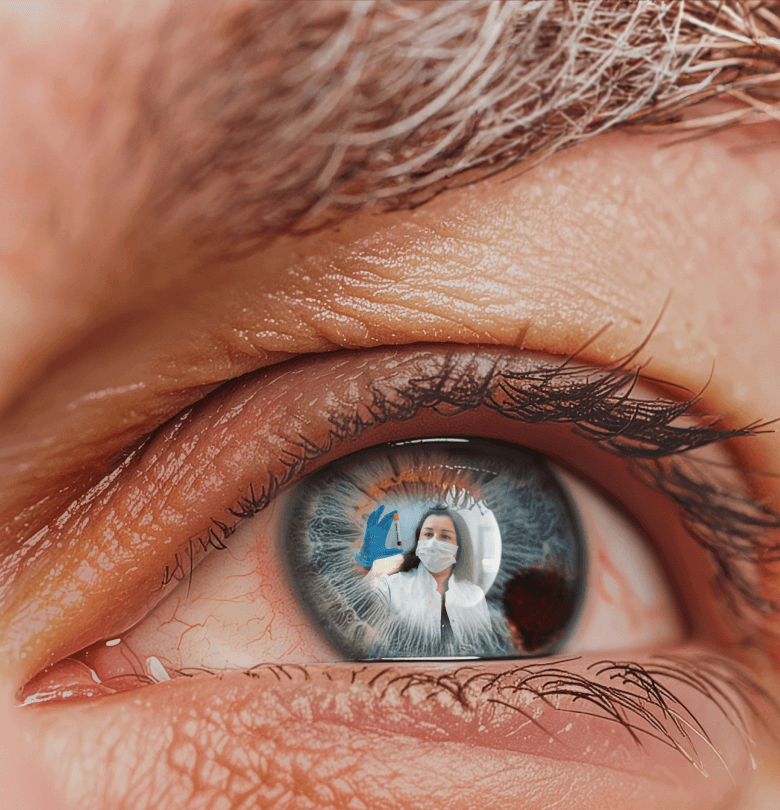


Metastatic Progression in Uveal Melanoma
It’s not just about what’s visible now, but what could be coming.¹
Early recognition of metastasis matters.¹
Risk Stratification today can define tomorrow’s path forward.2-5
Gene Expression Profiling MAY inform future decisions.3,4
Shared planning leads to optimal patient care.2
Early referral starts with you.
Metastatic Progression in Uveal Melanoma
It’s not just about what’s visible now, but what could be coming.1
Early recognition of metastasis matters.1
Risk Stratification today can define tomorrow’s path forward.2-5
Gene Expression Profiling MAY inform future decisions.3,4
Shared planning leads to optimal patient care.2
Early referral starts with you.
Don’t wait for symptoms. TESTING AND SURVEILLANCE should start early and be risk-informed.2-5
GEP/PRAME
Assist in shaping future care strategies with gene expression profiling AND PRAME TESTING3-5
In addition to tumor size and location, the genetic profile offers important information that can help assess metastatic risk and support informed decisions about future treatment options.2-4
Gene expression profiling (GEP) can reliably classify metastatic risk based on the tumor’s molecular profile.3,4
The addition of Preferentially Expressed Antigen in MElanoma (PRAME) testing to the GEP assay can provide more precise prognostic information and further refine the risk categories.3-5
CLASS 1A OR CLASS 1 PRAME (-)Low metastatic risk
CLASS 1B OR CLASS 1 PRAME (+)Medium metastatic risk
Class 2High metastatic risk
GEP AND PRAME TESTING can inform risk-adjusted patient management.3-5
FACTOR HLA BLOOD TESTING INTO THE LONG-TERM MANAGEMENT OF UM/mUM PATIENTS
When considering long-term treatment plans for UM patients at higher risk of metastasis, HLA testing may provide useful information.3 Genetic testing can determine treatment eligibility and support timely care decisions.3
Key points about HLA testing:
- HLA status is generally confirmed by a high‑resolution blood test (resolved to the fourth digit), which provides detailed allele group and the specific HLA protein6,7
- Tumor biopsy is not recommended for determining HLA status, as chromosomal changes in the tumor may affect results8,9
HLA Status can be assessed by a blood test at any time.10
Coordinated insight helps determine when and how to screen.2
Resources
Explore resources and clinical insights
All Eyes on Metastatic Risk in Uveal Melanoma
Hear leading ocular and medical oncologists discuss real-world approaches to risk assessment, surveillance, and long-term care in this expert roundtable series.
→ Upcoming roundtables and expert insights COMING SOON